It’s Saturday night right now and I can honestly say that since I woke up on Easter morning my life has been non stop for this entire week!
Of course, Easter was a wonderful way to start the week. I went to church, hung around after for breakfast, worked on a study guide when I got home, and then went with my roommate to her parent’s house for Easter dinner and an egg hunt. All together it was a great day and it was great to be able to spend time enjoying myself AND still prepare myself for this week of rotations.
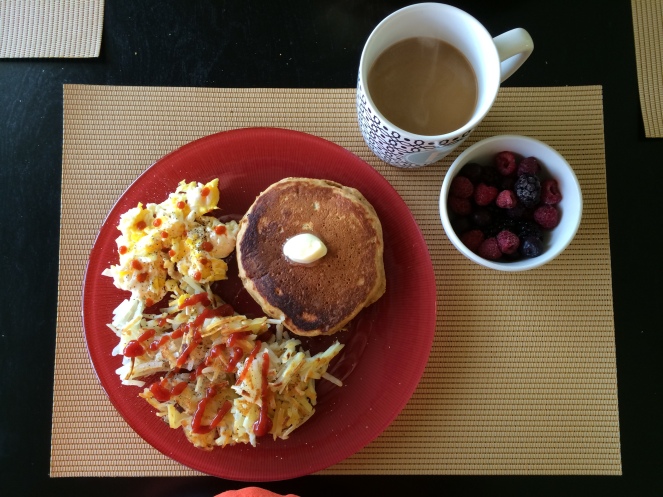
Oh, and my Easter started with this breakfast:
Pumpkin pancakes, eggs, hashbrowns, berries, and of course, coffee.
I wish I could eat breakfast like this every day!
Anyways, I spent this week of my hospital rotation in the intensive care unit (ICU). It was….an experience. I’m actually still going to be in there on Monday and Tuesday and I’ll have another week at the end of May so I’ll have 4 weeks total of experience in critical care (ICU and NICU) which is way more than I originally was scheduled to have.
I can’t decide if I really like critical care or not. One of the aspects of critical care that I really enjoy is how incredibly detail oriented it is. I really love details and I love tracking details. The critical care dietitians use what the hospital has named “visual management tools” (which is really just a fancy name to justify using a paper to track information instead of relying solely on the electronic medical record), so every morning starts with an in depth chart review of every patient the dietitian is following, usually anywhere from 7-12 patients.
They track everything from lab values, medications, and GI status (if they have a distended abdomen, are nauseous, etc.) to the amount of urine that is coming out of their foley catheter, the rate their tube feeding is running and the total amount they have had in a 24 hour period. They use the information they collect to make a snapshot of how the last 24 hours has gone for the patient and then decide what they want the patient to work on that day. Sometimes it’s increasing a tube feed rate, changing a tube feed formula, encouraging them to eat by mouth, or a number of other things.
I would say recognizing the big picture of what is happening with a patient is essential regardless of where in the hospital they are, but because of the critical care atmosphere it seems to be much more the focus of what is happening.
The entire care team rounds together every morning and it usually takes around 2 and a half hours to get to all 30 rooms on the floor and talk about what’s happening with each individual patient. Luckily, the dietitians only have to round on the patients they are following, which isn’t everyone, so it doesn’t take much more than an hour total. It’s so cool to see how everyone really works together as a team in the ICU and respects each others disciplines and opinions on the patient’s care.
The one thing I don’t really enjoy about the ICU is the lack of patient interaction. Many of the patients are intubated and sedated and are obviously in no position to be interviewed. A lot of time family is available but depending on the status of the patient and their outlook the families are often very emotional, distraught, and overwhelmed. To a lot of people it’s a very scary moment when the dietitian comes in and tells them that their loved one is going to start getting a tube feed. It takes a lot of explaining and educating the family about how a tube feed is incredibly beneficial to someone in the ICU who has a functioning gut and how it can help with their recovery in a tremendous way.
I love how important nutrition is in the ICU and how everyone values it as much as medicine, but it’s hard to have to read about the tragic events that have landed the patients in the ICU and even harder when you come in in the morning and realize the patient you spent an hour charting on the day before has passed away. Sometimes even the entire care team giving 110% to a patient isn’t enough to stop the inevitable.
I think I’ve learned more this week than I have in a long time, not just about nutrition, but about life. I’ve seen people get better, I’ve seen people die, and I’ve seen about every phase in between.
I feel very fortunate to be healthy, happy, in school, and moving forward with my career!